
Call for Appointment
+91 89709 34698
+91 97392 08007
+91 88800 41775
![]()
Consultation Timing
11:00 AM to 01:00 PM
04:00 PM to 07:00 PM
SUNDAY HOLIDAY

Call for Appointment
+91 89709 34698
+91 97392 08007
+91 88800 41775
![]()
Consultation Timing
11:00 AM to 01:00 PM
04:00 PM to 07:00 PM
SUNDAY HOLIDAY
English Version |
What Is Psoriasis?
Psoriasis is a long-lasting autoimmune disease which is characterized by patches of abnormal skin.
Psoriasis is a chronic autoimmune condition that causes the rapid build-up of skin cells. This build-up of cells causes scaling on the skin’s surface. Inflammation and redness around the scales are fairly common.
Typical psoriatic scales are whitish-silver and develop in thick, red patches. Sometimes, these patches will crack and bleed.
Psoriasis is the result of a sped-up skin production process. Typically, skin cells grow deep in the skin and slowly rise to the surface. Eventually, they fall off. The typical life cycle of a skin cell is one month.
In people with psoriasis, this production process may occur in just a few days. Because of this, skin cells don’t have time to fall off. This rapid, overproduction leads to the build-up of skin cells.
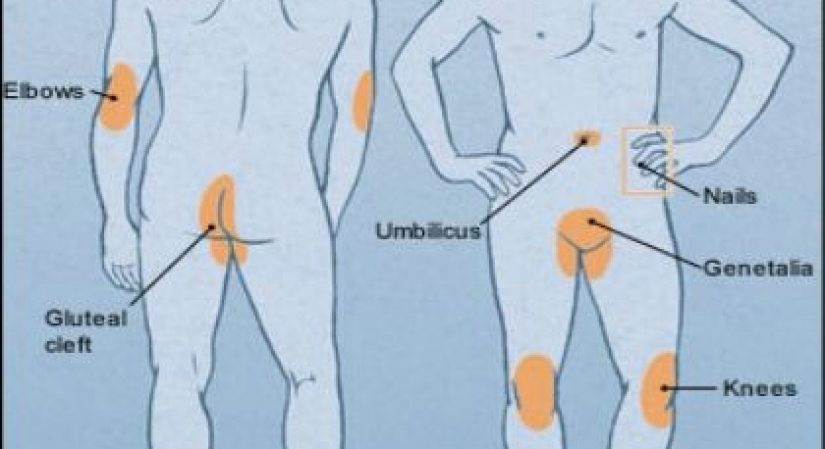
Scales typically develop on joints, such elbows, and knees. They may develop anywhere on the body, including the hands, feet, neck, scalp, and face. Less common types of psoriasis affect the nails, the mouth, and the area around genitals.
It’s commonly associated with several other conditions, including type 2 diabetes, inflammatory bowel disease, cardiovascular disease, and psoriatic arthritis.
Unpredictable and irritating, psoriasis is one of the most baffling and persistent of skin-disorders.
It’s characterized by skin cells that multiply up to 10 times faster than normal. As underlying cells reach the skin’s surface and die, their sheer volume causes raised, red plaques covered with white scales. Psoriasis typically occurs on the knees, elbows, and scalp and it can also affect the torso, palms, and soles of the feet.
What are the different types of psoriasis?
The 5 types of psoriasis and most common symptoms include:
Plaque psoriasis: This is the most common type of psoriasis — about 80 percent of people with the condition have plaque psoriasis. It causes red, inflamed patches that cover areas of the skin. These patches are often covered with whitish-silver scales or plaques. These plaques are commonly found on the elbows, knees, and scalp.
Guttate psoriasis: Guttate psoriasis is common in childhood. This type of psoriasis causes small pink spots. The most common sites for guttate psoriasis include the torso, arms, and legs. These spots are rarely thick or raised like plaque psoriasis.
Pustular psoriasis: Pustular psoriasis is more common in adults. It causes white, pus-filled blisters and broad areas of red, inflamed skin. Pustular psoriasis is typically localized to smaller areas of the body, such as the hands or feet, but it can be widespread.
Inverse psoriasis: Inverse psoriasis causes bright areas of red, shiny, inflamed skin. Patches of inverse psoriasis develop under armpits or breasts, in the groin, or around skin folds in the genitals.
Erythrodermic psoriasis: This type of psoriasis often covers large sections of the body at once and is very rare. The skin almost appears sunburned. Scales that develop often slough off in large sections or sheets. It’s not uncommon for a person with this type of psoriasis to run a fever or become very ill.
What are the symptoms of psoriasis?
Psoriasis symptoms differ from person to person and depend on the type of psoriasis. Areas of psoriasis can be as small as a few flakes on the scalp or elbow or cover the majority of the body.
The most common symptoms of plaque psoriasis include:
Not every person will experience all of these symptoms. Some people will experience entirely different symptoms if they have a less common type of psoriasis.
Most people with psoriasis go through “cycles” of symptoms. The condition may cause severe symptoms for a few days or weeks, and then the symptoms may clear up and be almost unnoticeable. Then, in a few weeks or if made worse by a common psoriasis trigger, the condition may flare up again. Sometimes, symptoms of psoriasis disappear completely.
What are the causes of psoriasis?
Scientists are unclear as to what causes psoriasis. However, thanks to decades of research, they have a general idea of two key factors: genetics and the immune system.
Immune system
Psoriasis is an autoimmune condition. Autoimmune conditions are the result of the body attacking itself. In the case of psoriasis, white blood cells known as T cells attack the skin cells mistakenly.
In a typical body, white blood cells are deployed to attack and destroy invading bacteria and fight infections. The mistaken attack causes the skin cell production process to go into overdrive.
The sped-up skin cell production causes new skin cells to develop too quickly. They are pushed to the skin’s surface, where they pile up.
This results in the plaques that are most commonly associated with psoriasis. The attacks on the skin cells also cause red, inflamed areas of skin to develop.
Genetics
Some people inherit genes that make them more likely to develop psoriasis. If you have an immediate family member with the skin condition, your risk for developing psoriasis is higher. However, the percentage of people who have psoriasis and a genetic predisposition is small. Approximately 2 to 3 percent of people with the gene develop the condition.
Psoriasis triggers:
Stress, alcohol, and more
External “triggers” may start a new bout of psoriasis. These triggers aren’t the same for everyone. They may also change over time for you.
The most common triggers for psoriasis include:
Stress: Unusually high stress may trigger a flare. If you learn to reduce and manage your stress, you can reduce and possibly prevent flares.
Alcohol: Heavy drinking or alcohol consumption can trigger psoriasis flares. If you binge drink or drink heavily, psoriasis outbreaks may be more frequent. If you have a problem with alcohol, talk with your doctor about getting help to quit drinking. Reducing alcohol consumption is smart for more than just your skin.
Injury: If you have an accident, cut yourself, or scrape your skin, you may trigger a psoriasis outbreak. Shots, vaccines, and sunburns can also trigger a new bout with the skin condition.
Medications: Some medications are considered psoriasis triggers. These medications include lithium, antimalarial medicines, and high blood pressure medication.
Infection: Psoriasis is caused, at least in part, by the immune system mistakenly attacking healthy skin cells. If you’re sick or battling an infection, your immune system will go into overdrive to fight the infection. This might start another psoriasis bout. Strep throat is a common trigger.
NAVAYAVVANA DISPENSARY
25/8, 1st Cross
Ground Floor
Sampige Apartment
Malleshwaram
Bangalore. 560003
Mob: +91 8880041775
EMAIL : info@roydoctor.com
Send Whatsapp
QUICK LINKS
BRANCH OFFICES
NAVAYAVVANA DISPENSARY
25/8, 1st Cross
Ground Floor
Sampige Apartment
Malleshwaram
Bangalore. 560003
Mob: +91 8880041775
Copyright © Navayavvana Dispensary, All Rights Reserved.